The healthcare landscape is complex, especially when it comes to billing for diagnostic tests. The Centers for Medicare & Medicaid Services (CMS) has specific guidelines that providers must follow to ensure compliance and avoid denials. This article by APEX Professional Solutions (aka The APEX Pros) aims to simplify these guidelines by highlighting key dos and don’ts when billing for diagnostic tests.
Do: Understand the Coverage Criteria
- Understand Local Coverage Determinations (LCDs): CMS coverage varies by region. It’s crucial to be familiar with the LCDs that apply to your area.
- Know the National Coverage Determinations (NCDs): These are CMS policies that apply nationally. Ensure your tests meet these criteria.
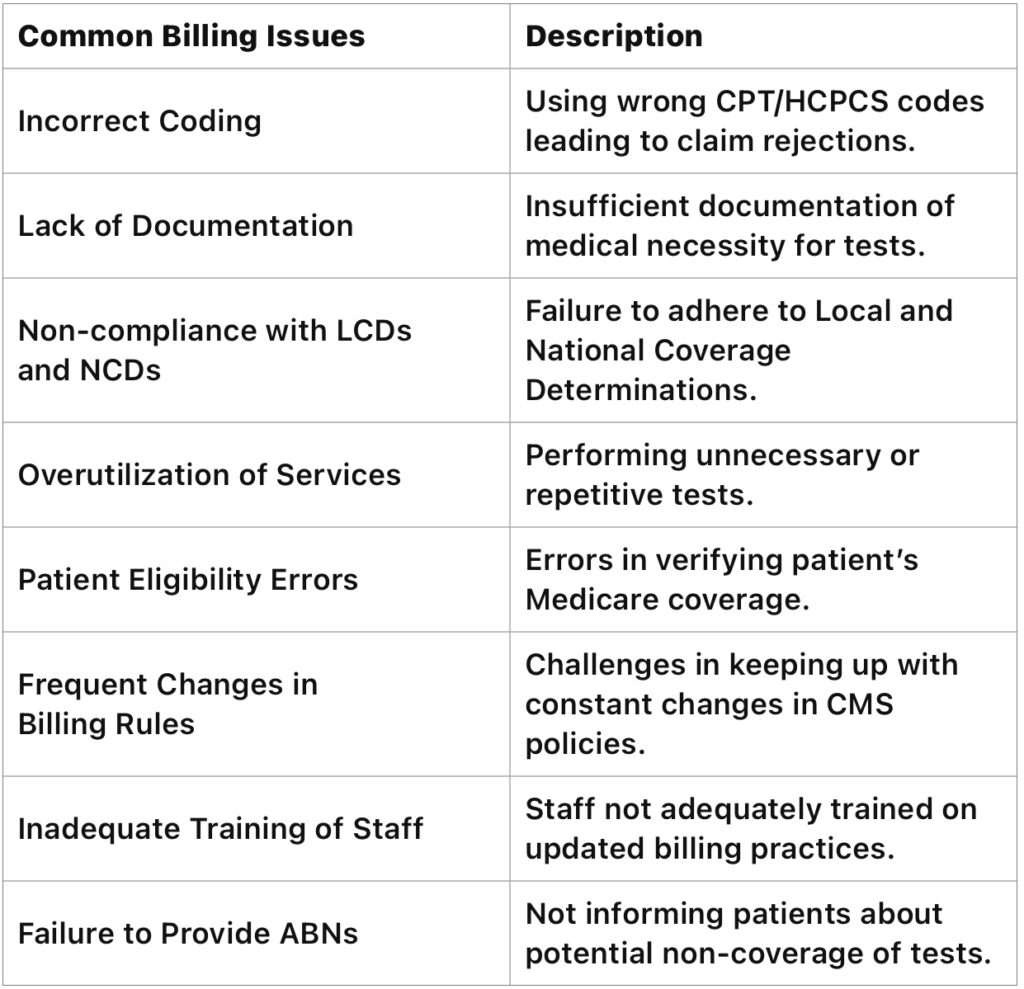
Do: Accurately Code Tests
- Use Correct CPT/HCPCS Codes: Assign the right Current Procedural Terminology (CPT) and Healthcare Common Procedure Coding System (HCPCS) codes. Incorrect coding can lead to claim rejections.
- Stay Updated on Coding Changes: Coding guidelines change frequently. Keeping abreast of updates is essential.
Do: Ensure Medical Necessity
- Document Medical Necessity: Clearly document why a test is medically necessary for the patient’s condition.
- Align Orders with Diagnosis Codes: The diagnosis must justify the need for the test. Mismatched codes can raise red flags.
Do: Be Mindful of Frequency Limitations
- Some tests have limits on how often they can be billed. Exceeding these limits without appropriate justification can result in denials.
Don’t: Ignore Beneficiary Notices
- Advance Beneficiary Notice (ABN): If a service might not be covered by Medicare, you must inform the patient using an ABN. Failing to do this can result in you bearing the cost.
Don’t: Perform Unnecessary Testing
- Avoid Overutilization: Conducting tests that aren’t necessary for the patient’s treatment or diagnosis is a violation of CMS guidelines.
Don’t: Misinterpret the Guidelines
- Assumptions Can Lead to Errors: Misunderstanding CMS guidelines can lead to incorrect billing, audits, and penalties.
Don’t: Forget About Compliance Training
- Regular training for staff on CMS guidelines and changes in billing practices is vital to maintain compliance.
Billing for diagnostic tests under CMS guidelines requires a careful approach. By adhering to these dos and don’ts, healthcare providers can avoid common pitfalls and ensure they remain compliant while providing necessary care to their patients. Let APEX Professional Solutions help you stay informed, as CMS guidelines can and do change, impacting how billing should be handled.
For a deeper dive into CMS guidelines, consider visiting the CMS website or consulting with a healthcare compliance professional. Remember, staying informed is key to successful and compliant billing practices in healthcare, and The APEX Pros are comprised of a trusted team of experts who can help you navigate the complex world of diagnostic billing. Contact us today to learn how we can your laboratory bill for your diagnostic specimens: info@theapexpros.com.